- Home
- Common Knee Conditions
- Plica Syndrome
Plica Syndrome
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board
Plica syndrome is a condition caused by inflammation in the lining of the knee joint.
It results in achy knee pain which gets worse with activity, particularly up and down stairs, a feeling of instability in the knee and sometimes a catching or locking sensation.
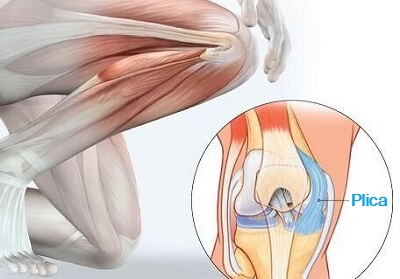
Plicae are small folds in the synovial membrane, the thin structure that surrounds and lines the knee joint. Plica syndrome, aka plica synovialis, can develop in any of the four knee plica, the most common being in the medial plica.
Knee plica irritation occurs when the plica gets caught or pinched between the knee bones, usually due to a knee injury or from overuse.
Here we look at how plica synovialis develops, the causes and symptoms, and finally look at the different treatment options for knee plica syndrome.
What Are The Knee Plica?
Knee plica are normal folds in the synovial membrane of the knee, a thin, fluid-filled capsule that encases the joint, like a bag. The word “plica” is Latin for “fold”.
During the first trimester of fetal development, connective tissue divides the knee into three compartments. During the second trimester, this tissue begins to reduce in size as the fetus starts moving more and is gradually reabsorbed before birth, leaving only a thin sleeve which surrounds the knee joint, the synovial membrane.
However, in up to 90% of the population, the connective tissue isn’t fully absorbed leaving small inward folds in parts of the synovial membrane, known as knee plica. Synovial plica are pliable and thin.
These folds in the membrane, known as synovial knee plica, are elastic so do not usually restrict normal knee movement and vary in size between individuals. In most cases, synovial plica are completely asymptomatic and don’t cause any problems. However, if the knee plica becomes irritated or inflamed, typically from overuse or an injury, plica synovialis develops causing pain and instability in the knee.
Causes Of Synovial Plica Syndrome
Plica syndrome develops when the synovial folds are irritated and become inflamed. This may be due to direct knee trauma, overuse or repetitive activities, or an underlying knee problem that affects the pliability of the synovial membrane.
The knee plica may get trapped or pinched between the knee bones, or caught on the femur. When this happens, the knee plica in question becomes inflamed, gradually thickens and eventually, if left untreated, becomes hard.
Plica syndrome is typically caused by:
- Direct Trauma: A blow to the knee e.g. a fall on to the knee or a RTA where the knee hits the dashboard
- Repetitive Knee Movements: Activities where you repeatedly bend and straighten the knee are often to blame for knee plica syndrome e.g. running, cycling, going up and down stairs
- Sudden Increase In Activities: If you rapidly increase your exercise levels it can lead to overloading of the synovial plica and thus they become inflamed
- Knee Injuries: particularly twisting injuries, meniscus tears or anything that causes bleeding in the knee joint
- Prolonged Flexion: sitting for long periods or sleeping with your knee bent often result in pain with plica synovialis
- Underlying Knee Conditions: such as osteochondritis dissecans, fat pad irritation or synovitis
- Muscle Weakness: As the plica are indirectly attached to the quadriceps, weakness in the quads muscles increases the force through the plica leading to irritation and inflammation
Symptoms Of Plica Syndrome
The symptoms of plica syndrome may develop suddenly with an injury, or gradually from overuse, in one or both knees. Typical symptoms of knee plica syndrome include:
- Knee Pain: Pain from plica syndrome tends to be dull and achy rather than sharp or stabbing. The location of the pain will depend on which plica is inflamed. Pain from plica synovitis is often worse at night time due to the build-up of inflammation
- Worse With Activity: activities where the knee bends and straightens such as going up and down stairs, squatting and getting in and out of chairs causes pain with plica syndrome
- Clicking or Popping Noises: when you bend and straighten your knee
- Knee Locking: It may feel like the knee catches or gets stuck at times, typically when you get up after sitting for a while
- Instability: People with plica synovialis often complain that their knee feels like it is going to give way, particularly when walking on slopes or up and down stairs
- Swelling: There may be localised swelling in the knee plica and/or the surrounding area
- Reduced Knee Movement: As the synovial plica thickens, it loses its elasticity which can restrict knee movements
Where Are Knee Plica Found?
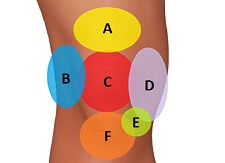
People may have up to four knee plica located in different parts of the knee, the medial plica, suprapatellar plica, infrapatellar plica and the lateral plica.
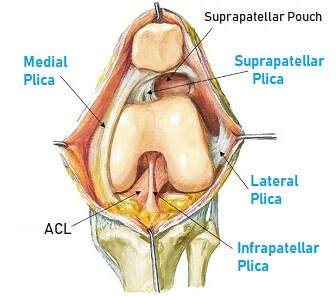
Plica syndrome can develop in any of these unless you are one of the 10% of the population have no knee plica at all.
1. Medial Plica
The medial plica is the most common place to develop symptomatic knee plica syndrome. It is found on the inner side of the knee joint, running parallel to the kneecap.
The medial plica runs from the bottom part of the knee cap on the medial side, over the medial femoral condyle and down to the synovial lining on the inner side of the tibia, where it blends with the ligamentum patellae and the infrapatellar fat pad. It is often referred to as being like a shelf.
The position of the medial plica makes it the most prone to getting caught in the knee joint resulting in medial plica syndrome, aka medial patellar plica syndrome, medial plica synovitis and plica synovialis mediopatellaris. This leads to inflammation and swelling in the medial plica and can cause a lump on the inside of the knee to form.
2. Suprapatellar Plica
The suprapatellar plica is found in the suprapatellar pouch, an area behind the kneecap extending up behind the quadriceps tendon. The suprapatellar plica is typically a domed, crescent shape, sitting between the suprapatellar bursa and the knee joint, and may be connected to part of the medial plica.
In some cases of suprapatellar plica syndrome, the plica becomes tethered with adhesions forming between the plica, the kneecap and the femoral condyle which can limit knee movement. It may feel like there is a lump above the knee.
Suprapatellar Plica Syndrome is also known as supramedial plica syndrome, superior plica and plica synovialis suprapatellaris
3. Infrapatellar Plica
The infrapatellar plica, aka ligamentum mucosum, may be shaped like a cord or bell-shaped. It sits inside the middle of the knee joint, alongside the Anterior Cruciate Ligament, attaching to the infrapatellar fat pad.
Whilst the infrapatellar plica is the most prevalent of the four knee plica, it does not tend to get damaged making infrapatellar plica syndrome rare.
Infrapatellar plica syndrome is also known as plica synovialis infrapatellaris.
4. Lateral Plica
The lateral plica is the least common of the four knee plica and is in fact, quite rare.
The lateral plica sits on the outer side of the knee, running down the lateral patella, and attaches to the infrapatellar fat pad.
Lateral plica syndrome is also known as plica synovialis lateralis or lateral para-patellar plica and can cause a lump on the outside of the knee.
Diagnosing Plica Synovialis
Knee plica syndrome is hard to diagnose as the symptoms mimic many other knee problems.
Your doctor will take a history asking questions about your knee pain. Plica syndrome is often diagnosed by ruling out other knee issues such as a meniscus tear or tendonitis.
To diagnose plica syndrome your doctor may do:

- Physical Exam: specific tests can be done to confirm or deny the presence of other knee conditions. Palpation of the medial plica will be painful with medial plica irritation, but it should illicit the specific symptoms rather than general tenderness.
There are also specific tests for plica syndrome such as the Plica Stutter Test and the Hughston Plica Test aka MPP test - X-rays: do not show up plica synovitis but can be helpful ruling out problems with the knee bones
- MRI Scan: An MRI scan is not normally indicated but may be used to help rule out soft tissue problems such as meniscus tears, ligament injuries or cartilage defects. Synovial plica are visible on MRI so the thickness and position of the plica can be assessed
- Arthroscopy: If plica syndrome is strongly suspected then keyhole surgery may be performed where a tiny fibre-optic camera is inserted into the knee so the surgeon can see the structures inside the joint
Treating Plica Syndrome
Treatment for plica syndrome focuses on reducing the inflammation in the synovial folds. Most people with plica synovialis will get better in 6-8 weeks with a course of physical therapy and will not require surgery.
#CommissionsEarned from Amazon on qualifying purchases
Treatment for knee plica syndrome normally involves a combination of:
- Rest: You should rest from aggravating activities such as cycling and running to allow the plica synovitis to settle down
- Ice: Regularly applying ice packs helps to reduce pain and inflammation
- Anti-Inflammatory Medication: NSAID’s such as ibuprofen/Advil can also help reduce pain and inflammation
- Stretching Exercises: Stretching the quadriceps and hamstrings helps to reduce the stress going through the knee plica - see knee stretches
- Strengthening Exercises: Strengthening the glutes, quads and VMO muscles helps take tension off the knee plica - see knee strengthening
- Corticosteroid Injections: If pain is stopping you from exercising, your doctor may give you a steroid injection into the synovial plica to reduce the pain and inflammation so that you can start rehab. Injections should not be used in isolation as they only temporarily improve symptoms
- Physical Therapy: treatment will be tailored to your situation and will look at patellofemoral tracking and alignment, foot biomechanics and balance and proprioception. They will also give you a programme of strengthening and stretching exercises
If you are getting a lot of pain at night-time from plica synovialis, it can help to sleep with a pillow or duvet in between your knees.
Surgical Treatment
If the symptoms of plica syndrome fail to settle after 3-6 months of non-surgical treatment, then your doctor may advise surgery.
Surgery for plica syndrome will be carried out arthroscopically – key hole surgery. Small incisions are made around the knee joint and a fibre-optic camera is inserted into the knee so the surgeon can fully evaluate the joint.
Small surgical tools are used to remove the inflamed plica, known as synovial plica resection. The surgeon will also inspect the integrity of the other structures in the joint and may also carry out a meniscectomy, if there is a tear in the cartilage, or a lateral release, if the lateral retinaculum is tight.
A course of physical therapy is recommended after synovial plica resection surgery to prevent scarring and ensure full recovery. Physical therapy will be very similar to that with non-surgical management aiming to improve knee strength, motion and function and reduce any swelling.
Recovering From Plica Syndrome
Recovery from plica syndrome will depend on a number of factors – the age of the patient, how long they’ve had symptoms, which plica is affected, compliance with physical therapy and whether there are other associated knee problems.
The best outcomes are usually achieved in younger patients who have only had symptoms of plica synovitis for a short time.
Differential Diagnosis
There are a number of other knee conditions that present in a similar way to knee plica syndrome:
- Patellofemoral Pain Syndrome aka Runners Knee
- Chondromalacia Patella
- Osteochondritis Dissecans
- Bursitis
- Meniscus Tears
- Bipartite Patella
- Ligament Sprain
- Patellar Tendonitis
- Arthritis
- Swelling Above The Knee
- Swelling On Side Of Knee
If you have been treated for any of the conditions above and your symptoms have failed to improve, it may well be that knee plica syndrome is to blame.
Related Articles
References
1. Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain. By P. Feng Lee, A. Nixion and J. M. Murray. The Surgery Journal. February 2017
2. The Role of Complete Suprapatellar Plicae. By T. Mine, K. Chagawa, K. Ihara, H. Kawamura, R. Kuriyama & R. Date. Arthroscopy Techniques Journal. February 2016
3. MR Imaging of Infrapatellar Plica Injury. R. Cothran, P. McGuire, C. Helms, N. Major & D. Attarian. American Journal of Roentgenology. May 2003
4. Anatomy and MR Imaging Appearances of Synovial Plicae of the Knee. R. García-Valtuille, F. Abascal, L. Cerezal, A. García-Valtuille, T. Pereda, A. Canga & A. Cruz. Radiographics. July 2002
Page Last Updated: December 12th, 2024
Next Review Due: December 12th, 2026